Myoguide System Training
EMG Guided Injection System Animation
The Myoguide system is designed to amplify EMG signals from muscle and provide audio feedback to assist clinicians in locating areas of muscle activity. Clinicians can see and hear EMG activity. Treatment delivery can be in the form of neuromodulator injections such as Botox©. Applications include management of spasticity (Movement Disorders), and cosmetics. The “Quick Start” animated video illustrates many aspects of Myoguide operation.
Myoguide is currently SOLD OUT!
EMG Guidance helps find the target
There are many compelling reasons to use EMG guidance. The first is that EMG ensures that the needle is located in a muscle and in a muscle that is actively contracting in association with the disorder. Speelman and Brans (Cervical dystonia and botulinum treatment: is electromyographic guidance necessary? (Letter). Mov Disor 1995;10(6):802) showed that even the most experienced “blind” injectors were frequently inaccurate in identifying needle placement in muscles of the neck. The error rate ranged from 15% in an easily palpated superficial cervical muscle, such as sternocleidomastoid, to greater than 50% in deeper muscles, such as levator scapulae and semispinalis capitis (] Dressler D. Botulinum toxin therapy. New York: Theime Stuttgart; 2000). Comella and colleagues (Botulinum toxin injection for spasmodic torticollis: increased magnitude of benefit with electromyographic assistance. Neurology 1992;42:878–82), in the only published study comparing experienced investigators using EMG versus palpation, showed that EMG was superior in terms of reducing side effects and obtaining clinical benefit. Recent studies showed that both expert and novice needle placements improve with guidance when compared without, even in large easily accessible muscles. (Manual Needle Placement: Accuracy of Botulinum toxin A Injections; October 2012; Muscle and Nerve 46 531-534; Alexis Schnitzler, MD, Nicholas Roche, MD, Philippe DeNormandie, MD, Christine Lautridou, MD, Bernard Parratte, MD, PhD, and Franc Ois Genet, MD).
A recent review article by Grigoriu et al., showed strong evidence that instrumented guided injections including Ultrasound, EMG and STIM, were more effective than manual needle placement for the treatment of spasmodic torticollis, and both upper and lower limb spasticity. (Grigoriu AI, Dinomais M, Rémy-Néris O, Brochard S. Impact of Injection-Guiding Techniques on the Effectiveness of Botulinum Toxin for the Treatment of Focal Spasticity and Dystonia: A Systematic Review. Arch Phys Med Rehabil. 2015 Nov;96(11):2067-78.e1. doi: 10.1016/ j.apmr.2015.05.002. Epub 2015 May 14.PMID: 25982240 )
These studies clearly illustrate that we all do better finding the optimal spots to locate the needles when using EMG guidance, regardless of whether the muscle is located easily on the surface, or deeper, or whether the needle insertions are being carried out by novice or experts. Myoguide can be used to improve patient outcomes by improving accuracy.
Best Electrode Practices
Please have a look at our Blog post about EMG Guidance
Guidance procedures require a quality hypodermic needle electrode and two surface electrodes. The needle electrode plugs into the black connector. One surface electrode is connected to the green connector and is for the ground, and the other connects to the red connector and is for the reference. We would like to present the following guidelines to ensure you have the best possible situation for measuring great EMG signals from the hypodermic needle electrode to support your injection guidance procedures. The hallmark we all need to embrace is that we need “Fresh Surface Electrodes!” “oldies are not goodies”. Avoid using surface electrodes that have been sitting in an open package laying around without any knowledge of when the package was opened. Surface electrodes will keep for a 2-3 weeks once the foil package has been opened. Please don’t use old electrodes, as they will affect the quality of the EMG signal and the ability to deliver stimulation. Let’s address the placement of the surface electrodes to help us collect the best possible signals. Some simple pre-planning will gain best results for the entire procedure if one area is being treated. These simple principles will help you create the best opportunities to collect great signals:
- No real need to move the reference and ground electrodes if all the injection sites are close by.
- Most times only the reference electrode needs to be moved if there are bilateral injections.
- Avoid placing electrodes in areas that will see ultrasound goop! This will avoid short circuits and peeling surface electrodes.
Finer Points
Please have a look at our Blog post about EMG Guidance
Myoguide’s EMG bandwidth is tuned to record the highest density of EMG spectral elements. Myoguide can measure a range of 10-700Hz and the audio section can produce high fidelity sounds that range from 20-700Hz. This is creates the best possible EMG audio within the range of the most important EMG spectral elements needed for aural identification of EMG. This provides the clinician with EMG audio similar to what is heard on full size EMG systems. Exclusive feature “Audio Mute” allows the clinician to easily silence the EMG audio. Audio will be returned to the pre-muted level with a touch of any button
Myoguide is equipped with what is essentially a single channel EMG machine with a full featured, built in stimulator.
Myoguide’s stimulator presents 5 stimulation frequency choices, four pulse width choices, and 1- 20 mA of stimulation current available in both 1 mA and 0.1 mA steps.
0.1 mA steps are helpful and necessary for nerve location procedures allow evoking responses at lower, more comfortable stimulation levels. This capability is the latest update for Myoguide and available as an upgrade for any Myoguide device currently only capable of 1.0 mA steps. Please contact us for details about our upgrade program.
Pulse widths of up to 500 microseconds allow evoking muscle twitches at lower currents, yielding a more comfortable clinical experience for patients undergoing stimulation location procedures.
Wider stimulation choices allow evoking twitch at lower, more comfortable stimulation levels.
Exclusive feature, “Stimulation Pause” allows clinicians to easily halt the stimulation process. This is especially useful when repositioning the injection needle electrode in order to fine tune its location for a more accurate injection point. Stimulation can easily be returned to the pre-paused current level with the touch of any button.
Feel free to browse our website, or view YouTube videos on the “intronixtech” channel, to see Myoguide in action in both clinical and animated videos.
Please have a look at our Blog post about EMG Guidance
EMG may, or may not, be present when the hypodermic needle is inserted. Here are a few possible scenarios:
- Needle insertion may result in transient insertional activity, resulting in a transient EMG signal that will disappear.
- Needle insertion may result in spontaneous continuous EMG
- Needle insertion may result in no spontaneous EMG signals. (If this is the case, confirmation of the muscle target must be confirmed and isolated, by patient initiated movement and/or specific manual manipulation to activate the muscle, using patient engagement and resistance to movement to initiate EMG signals)
Nerve stimulation with a low-intensity electrical current has become a vital part of the performance of peripheral nerve blockade.
How does the Myoguide Injection Guidance system stand up to the accuracy and characteristics of peripheral nerve stimulators used in clinical practice in the United States and Canada?
All peripheral nerve stimulators perform uniformly well when set to deliver currents of 1.0 mA or more. Lower currents of all peripheral nerve stimulators tend to have a higher median error.
The same is true for pulse width accuracy ranges. As far as the ability to ensure proper delivery of higher currents, this is up to the available compliance voltage. This is the voltage that is available to generate the proper constant current level for a given load.
Myoguide has one of the highest levels of compliance, which is up to 300 Volts. While this is more essential for ESTIM guidance, Myoguide will never run out available overhead for lower constant current stimulation levels.
Myoguide specifications compare well with any dedicated peripheral nerve stimulator.
Myoguide will deliver:
- OUTPUT CURRENT: 0– 20mA; adjustable in 1.0 mA or 0.1 mA steps
- Current less than 2mA: Average error > 30%
- Current more than 2mA: equal or less than displayed current within 10%
- STIMULATOR FREQUENCY:1,3,5,7, or 10 Hz +/- 5%
- PULSE WIDTH: 50, 100, 200, or 500 μs pulse width +/- 1%
- OUTPUT WAVEFORM: Monopolar square waveform
- ELECTRODE IMPEDANCE: 200 – 10 kΩ
- MAXIMUM EXCITATION: 300V
Use of Myoguide as a Peripheral Nerve Stimulator
The setup for Myoguide use as a peripheral nerve stimulator is fairly simple.
- The black Input/Output connector, in this case “output” connector, connects to the needle electrode to be used for delivery of the pulse
- The Reference (red) connector (surface electrode) is needed in order to generate the stimulation pulse.
These electrodes should be located close together, or strategically placed if multiple stimulation points are needed, so the reference won’t have to be moved.
- The ground (green) connector must be used to ensure a secure ground.
Myoguide will always default to EMG mode, when you turn it on. You need to get into STIM mode by holding the MODE button until you’ll hear the relay click and the “Stimulating" screen is shown.
- The unit will default to 0.0mA and be in the 1.0mA step mode. Once you start increasing the stimulation from 0.0, you will see the yellow stimulation light illuminate to indicate the stimulation is live and actively working.
- If you want to advance in 1.0mA steps and then fine tune with 0.1mA steps, you just need to move the left/right arrow buttons to highlight the 0.1mA side and use the up/down arrow buttons to modify the stimulation in 0.1mA steps.
- You can select the stimulation frequency and pulse width, by moving the left/right arrow buttons to highlight these parameters and then the up/down arrows to increase or decrease your selection of pulse width and stimulation frequency.
- Use the left/right arrow buttons to move the cursor to the current selection area. You will probably want to use the left/right arrow buttons to move the cursor to the .0 side of the mA symbol, to be in 0.1mA step mode. You will then be able to stimulate.
- The stimulation pause function: You can pause the stimulation at any time, by simultaneously pressing the left/right arrow buttons. You can see the pause symbol above these. This will stop the stimulation and you will see the stimulation light turn off. You can restart stimulation at the last stimulation setting, by simply pressing any button, and it will restart stimulating at the last setting.
Please explore all this functionality with your Myoguide, using surface electrodes on your hand, to help become more familiar with the process, before delivering treatment to your patients. The exercise will build confidence and help streamline your approach for patient encounters (see Test Drive Your Myoguide).
References
Greenblatt GM, Denson JS: Needle nerve stimulator locator. Nerve blocks with a new instrument for locating nerves. Anesth Analg 1962;41:599–602.
Montgomery SJ, Raj PP, Nettles D, Jenkins MT: The use of the nerve stimulator with standard unsheathed needles in nerve blockade. Anesth Analg 1973;52:827–831.
Ford DJ, Pither CE, Raj PP: Electrical characteristics of peripheral nerve stimulators: Implications for nerve localization. Reg Anesth 1984;9:73–77.
Pither CE, Ford DJ, Raij PP: The use of peripheral nerve stimulators for regional anesthesia, a review of experimental characteristics, technique, and clinical applications. Reg Anesth 1985;10:49–58.
Andres, J.A., Vila, M., Bolinches, R.T., & Serrano, M.T. (1988). Use of a peripheral nerve stimulator in regional anaesthesia : clinical evaluation.
Admir Hadzic, Jerry Vloka, Nihad Hadzic, Daniel M. Thys, Alan C. Santos; Nerve Stimulators Used for Peripheral Nerve Blocks Vary in Their Electrical Characteristics. Anesthesiology 2003; 98:969–974
Hadzic A, Vloka JD, Claudio RE, Thys DM, Santos AC: Electrical nerve localization: Effects of cutaneous electrode placement and duration of the stimulus on motor response. Anesthesiology 2004;100:1526–1530.
Kaiser H, Neuburger M: How close is close enough—How close is safe enough? Reg Anesth Pain Med 2002;27:227–228.
Bollini, C.A., & Cacheiro, F. (2006). Peripheral nerve stimulation. Techniques in Regional Anesthesia and Pain Management, 10, 79-88.
Neuburger M, Rotzinger M, Kaiser H: Electric nerve stimulation in relation to impulse strength. A quantitative study of the distance of the electrode point to the nerve. Acta Anaesthesiol Scand 2007;51:942–948.
Bosenberg AT, Raw R, Boezaart AP: Surface mapping of peripheral nerves in children with a nerve stimulator. Paediatr Anaesth 2002;12:398–403.
Urmey WF, Grossi P: Percutaneous electrode guidance. A non-invasive technique for prelocation of peripheral nerves to facilitate peripheral plexus or nerve block. Reg Anesth Pain Med 2002;27:261–267.
Urmey WF, Grossi P: Percutaneous electrode guidance and subcutaneous stimulating electrode guidance. Modifications of the original technique. Reg Anesth Pain Med 2003;28:253–255.
Capdevilla X, Lopez S, Bernard N, et al: Percutaneous electrode guidance using the insulated needle for prelocation of peripheral nerves during axillary plexus blocks. Reg Anesth Pain Med 2004;29:206–211.
Tsui BC, Gupta S, Finucane B: Confirmation of epidural catheter placement using nerve stimulation. Can J Anesth 1998;45:640–644.
Tsui BC, Guenther C, Emery D, Finucane B: Determining epidural catheter location using nerve stimulation with radiological confirmation. Reg Anesth Pain Med 2000;25:306–309.
Tsui BC, Kropelin B: The electrophysiological effect of dextrose 5% in water on single-shot peripheral nerve stimulation. Anesth Analg 2005;100:1837–1839.
Tsui BC: Electrical impedance to distinguish intraneural from extra-neural needle placement in porcine nerves during direct exposure and ultrasound guidance. Anesthesiology 2008;109:479–483.
Urmey WF, Grossi P: Use of Sequential Electrical Nerve Stimuli (SENS) for location of the sciatic nerve and lumbar plexus. Reg Anesth Pain Med 2006;31:463–469.
Jochum D, Iohom G, Diarra DP, Loughnane F, Dupré LJ, Bouaziz H: An objective
assessment of nerve stimulators used for peripheral nerve blockade. Anesthesia 2006;61:557–564.
Slavin, K.V. (2011). Peripheral nerve stimulation for neuropathic pain. Neurotherapeutics, 5, 100-106.
Klein, S., Melton, M.S., Grill, W.M., & Nielsen, K.C. (2012). Peripheral Nerve Stimulation in Regional Anesthesia. Regional Anesthesia & Pain Medicine, 37, 383 - 392.
Banks, G.P., & Winfree, C.J. (2019). Evolving Techniques and Indications in Peripheral Nerve Stimulation for Pain. Neurosurgery clinics of North America, 30 2, 265-273 .
Myoguide Power: Alkaline Versus NiMH Rechargeable Batteries
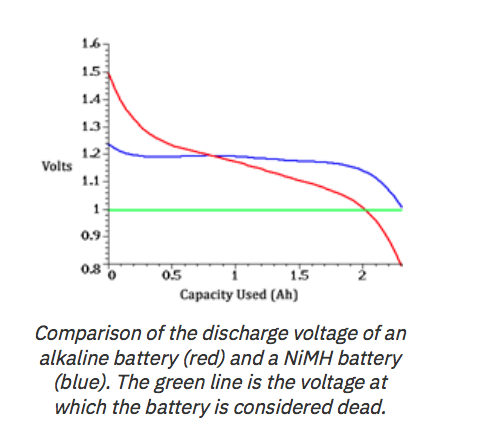
Even though the NiMH rechargeable batteries have a lower specified capacity (2300mAH) and lower voltage (1.2V) compared to a typical Duracell ProCell Alkaline AA battery (2850mAH, 1.5V), they tend to provide more capacity in a higher current draw situation.
NiMH rechargeable batteries provide a more steady discharge than an alkaline battery. i.e. Alkaline batteries have a steeper discharge curve as the load current requirements increase.
The downside to using a NiMH rechargeable in the Myoguide is that the battery display icon is calibrated for a 1.5V (Alkaline) battery and hence when using NiMH rechargeables, the battery icon will only display ¾ full when the NiMH are at full charge and will show empty when batteries are 50% discharged. i.e. The unit will run for quite a considerable time when the battery icon shows empty
Note: Due to the fact that battery discharge is not linear (logrhythmic) and the battery detection circuit is designed to linearly display the current battery voltage, the display is not a truly accurate rendition of the state of charge. i.e. when the display shows one bar, there still may be considerable battery capacity remaining. The batteries should be replaced when the display indicates “ Battery Low!”
Battery test comparison
Test 1:
80% EMG mode with 200Hz, 1mVp-p signal in, Vol:4.
20% Stimulation @ 1mA, 500uS pulse width, 1 Hz frequency into a 10 KOhm load
Alkaline batteries (Duracell MN1500): 8 Hr. 20 min.
Alkaline batteries (Duracell ProCell PC1500): 8 Hr. 10 min.
NiMH Rechargeable (Energizer NH15): 14 Hr. 39 min.
Test 2:
Constant Stimulation @ 4mA, 500uS pulse width, 1 Hz frequency into a 10 KOhm load
Alkaline batteries (Duracell MN1500): 3 Hr. 5 min.
Alkaline batteries (Duracell ProCell PC1500): 2 Hr. 15 min
NiMH Rechargeable (Energizer NH15): 4 Hr. 35 min
Test 3:
Constant Stimulation @ 1mA, 500uS pulse width, 1 Hz frequency into a 10 KOhm load
Alkaline batteries (Duracell MN1500): 3 Hr. 33 min
Alkaline batteries (Duracell ProCell PC1500): 3 Hr. 6 min
NiMH Rechargeable (Energizer NH15): 5 Hr. 17 min
Test 4:
80% EMG mode with 200Hz, 1mVp-p signal in, Vol:4.
20% Stimulation @ 4mA, 500uS pulse width, 1 Hz frequency into a 10 KOhm load
Alkaline batteries (Duracell MN1500): 7 Hr. 47 min.
Alkaline batteries (Duracell ProCell PC1500): 7 Hr. 35min.
NiMH Rechargeable (Energizer NH15): 9 Hr. 33 min.
Conclusion:
NiMh rechargeable battery use in the Myoguide unit provides considerably more run time compared to disposable alkaline batteries. This is especially true when the unit heavily used in Stimulation Mode.
Myoguide Loaner Programs
Myoguide Inc. is now offering our own Myoguide loaner program, which provides Myoguide units for trial, to qualified clinicians, as part of our commitment to injection training and support. Physicians have an opportunity to demo the Myoguide™ system in their clinic, to practice muscle localization for therapeutic toxin injections. Systems are available for a 30-day free trial (shipping not included).
Simply fill out the Myoguide loaner form and contact Myoguide Inc. with your request at support@myoguide.com and a representative will contact you directly. We advise all participants to contact us for online training before engaging patients. We believe this is a great way to learn and pick up useful tips before your first guided injection patient encounter.
Allergan USA offers a Myoguide loaner program to customers as part of its commitment to injection training and support. Physicians can have an opportunity to demo the Myoguide™ system in their clinic, and use it to practice muscle localization for injection. Systems are available free of charge for 1 month. Contact your Allergan Representative about Myoguide™ unit availability. The Intronix website and iNFOcard provide comprehensive training resources including how to operate Myoguide, however, we are available at our toll-free number, or by Email, should anyone have any questions about Myoguide operation or best practices.
Benefits to Using the Loaner Program
- Practice using EMG for muscle selection and injection in your own clinic
- Demo an EMG unit without large capital commitment
- Ability to purchase a Myoguide™ system with Allergan preferred pricing
At the end of Allergan’s 30 day period, the Myoguide™ system must be returned to MedForce via a pre-paid FedEx Label which your Allergan Representative will provide during delivery.
For more information, click here to read the brochure (PDF format).
Need more training? Please contact us for a WebEx, ZOOM, or Microsoft Teams based training session to review Myoguide operation and live Q & A.
Hands- On: Learning to Use Myoguide
The following steps can be used to learn and verify functionality of the Myoguide device.
For first time users, it is a good idea to play with Myoguide on your own, before engaging patients. These exercises will help you learn about measuring EMG and delivering stimulation on your own hand, using surface electrodes. It’s a simple way to learn to use Myoguide without a patient.
This procedure can also be used when experiencing perceived issues related to excess noise or stimulator performance. If perceived issues have been eliminated using the following procedure, the functionality of the Myoguide device can be confirmed and sources of perceived issues can be focussed on electrode quality, electrode placement or proper skin preparation.
Myoguide Set-up Procedure
1.0 Application and setup of electrodes
Using the photo as a guid
If using leaded surface electrodes, the surface electrode leads can be plugged directly into the Myoguide Input Cable (Model 8008-CT) with red surface electrode connector plugged into red connector on Myoguide input cable, black surface electrode plugged into black connector on Myoguide input cable and green surface electrode connector plugged into green connector on Myoguide input cable.
Tab or Snap type surface electrodes can alternately be used by using the supplied colour coded Myoguide cable adapters (Model 8008-CA, Model 8008-CA-R and Model 8008-CA-G). Simply connect the cable adapters to the corresponding coloured jacks on the Myoguide Input Cable and clip the alligator connector end to the surface electrode tab or snap.
Leaded electrodes should be as short as possible, to avoid extraneous noise pick up from the unshielded high impedance lines. This is true for both this learning exercise, as well as clinically.
When long lines are unavoidable in the clinic, you can reduce noise by eliminating noise sources like fluorescent lights. Noise can also be reduced by twisting the leads, that will wrap the ground wire around the input and reference inputs. This will act as a makeshift shield.
Please clean the skin area where surface electrodes are to be applied using proper skin preparation techniques and apply the electrodes as shown.
NOTE: Surface electrodes must be from an un-opened, non-expired package. As surface electrodes have a shelf life, use of expired or dried out/stale electrodes can cause noise and performance issues which will be seen as excessive noise or failure to display EMG correctly or degraded stimulator performance.
2.0 EMG Mode Verification
Turn on the Myoguide and set the Vol: parameter to 4 (default setting) and the V: parameter to 2.
The volume setting is actual the amplifier’s gain control. The “V” parameter is simply a visual display control.
Myoguide should now display EMG with minimal display deflection when the thumb is at rest and clean larger EMG deflection when thumb is flexed. If this is observed, the device is functioning correctly in EMG Mode.
3.0 Stimulation Mode Verification
To verify Stimulation Mode functionality, press and hold the Mode button on the device until the Stimulation screen is displayed. Set F: parameter (Frequency) to 1 Hz and PW: parameter (Pulse Width) to 500uS. Position the cursor over to the leftmost digit of the mA parameter (adjusts stimulation current by 1mA per step).
Slowly increase the Stimulation current until stimulation is felt in the thumb. Typically, stimulation becomes quite pronounced by 5 or 6 mA. If Stimulation is felt, the device is functioning correctly in Stimulation Mode.
Please play around with the stimulation pulse widths, and you should notice that wider pulse widths can evoke a twitch at a lower current setting. This should be more comfortable for you and subsequently for your patients.
If correct functionality is determined using the above procedure, issues related to noise, movement artifact and stimulation performance are most likely related to electrode quality, sub-optimal electrode placement or skin preparation.
Feel free to contact us if there are any questions. We will be happy to respond and help you with learning to use Myoguide, or solving any performance issues.
Please find the model numbers and descriptions for all Myoguide unit input cable and adapter cables (touchproof to alligator)
| 8008-CT Myoguide Main Input Cable (Input guarded shield)
This is the standard length (28”/ 71cm) main input/output cable, that was originally supplied, (white with colour coded connectors) that has 3 touchproof connectors (DIN 42-802 Type BU-UL-94 VO). |
| 8008-CT15 Myoguide, Extended Length, Main Input Cable (Input guarded shield)
This is the extended length (42”/ 107cm) main input/output cable (white with colour coded connectors) that has 3 touchproof connectors (DIN 42-802 Type BU-UL-94 VO). |
| 8008-CA-R Input Cable Adapter - Red
This is the red touchproof to alligator connector adapter that was originally supplied (DIN 42-802 Type ST) |
| 8008-CA-G Input Cable Adapter - Green
This is the green touchproof to alligator connector adapter that was originally supplied (DIN 42-802 Type ST) |
| 8008-CA Input Cable Adapter - Black
This is the black touchproof to alligator connector adapter that was originally supplied (DIN 42-802 Type ST) |
Cleaning and Disinfection:
Recommendations for cleaning and disinfecting Myoguide units are included in the Myoguide Instruction Manual, as well as, on the Myoguide iNFOcard included with every Myoguide purchased.
We suggest wiping Myoguide units with a minimum of 70% alcohol, or use of non-phenol disinfectant wipes (Phenols damage plastic), such as: Optim 33TB wipes (SciCan).
We find that Myoguide button panels can be damaged from continuous use of phenol disinfectants. If your button panel is damaged, you may purchase a button panel replacement kit from the Myoguide store. Button panels may easily be replaced by users, following simple instructions. Please call, or use the "contact us" form, found on this website, for more information
Myoguide Key Panel Replacement
( Available from the Myoguide Store)
- Gently remove old key panel using small blade/ knife, being careful not to scratch the surface of the device.
- Remove any remaining label backing and adhesive from the unit enclosure using isopropyl alcohol (This is an essential step)
- Let unit dry
- Once Chassis is dry, peel backing off of new panel and apply to the unit
- Verify that new panel operates correctly by powering unit on and verify all buttons perform their desired functions.
If you require assistance or have any questions, please contact us.